The Role of AI in Pathogen Detection and Epidemic Prediction

AI in pathogen detection: techniques and advancements
Modeling epidemics: AI’s predictive power
Challenges and limitations of AI in disease detection
Case studies: AI in action against recent outbreaks
The future of AI in epidemiology
Ethical considerations and data privacy
Conclusion
References
Further reading
AI is a rapidly expanding and vibrant area of technological development with applications in a vast array of disciplines. From drug discovery to language processing to general pattern recognition, this integration of human intelligence into machinery demonstrates the widespread applicability of large-scale data analysis.1

White medical masks and respirators with glove, hand sanitizer on blue background. Image Credit: Igisheva Maria/Shutterstock.com
Over the past three years, a new application of AI has become increasingly more relevant and apparent. With the outbreak of the COVID-19 pandemic, attention began to focus on how AI could improve public health, specifically pathogen detection and epidemic prediction.1-6
Epidemics and pandemics often outpace authorities, spreading at significant levels before experts are aware they exist at all.3 Introduction of AI, in addition to traditional surveillance methods, can lead to earlier detection of pathogen spread, decreased strain on human resources, especially in low-income countries, and improved recommendations on proactive measures.3
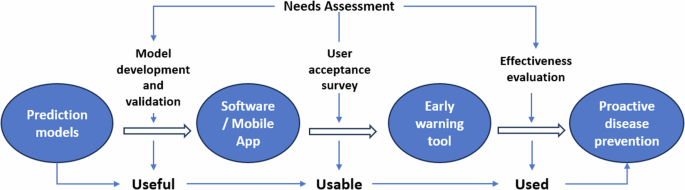
Harnessing artificial intelligence for infectious disease prevention
AI in pathogen detection: techniques and advancements
The flexible and non-linear nature of pathogen activities lend themselves to AI-based approaches. Machine Learning (ML) represents a subfield of AI devoted to developing decision-making systems trained on sample data.4 In epidemic prediction, ML can use real-time data to improve understanding of daily exposure behavior, separate risk groups, and assess viral availability to geographic locations.4
Neural Networks (NNs) represent another subfield of AI concerned with further mimicking information absorption in the human brain by combining multiple algorithms simultaneously.4 NNs have become incredibly valuable in pathogen detection, particularly in assessing interactions of disease transmission, expansion, and causation. 4
Pathogen and outbreak detection generally require four elements: natural language processing of open-source data, identification of regional signal patterns, modeling of outbreak behaviors, and rapid identification of misinformation. 3
Using these criteria, ML methods have demonstrated the ability to improve the prediction of mortality risk and diagnosis of COVID-19, forecast near-future infection rates, and identify symptoms of long COVID.4 Outside of the COVID-19 pandemic, sequence-guided approaches have been developed successfully in the prediction of pathogen immune system escape patterns for HIV-1 and influenza.7,8
Modeling epidemics: AI’s predictive power
To successfully forecast and model epidemics, AI platforms require an extensive list of data. This includes case counts (confirmed, probable, suspected), mobility of individuals and populations, host susceptibility (immunization coverage data), environmental susceptibility (climate temperature, precipitation, etc.), healthcare capacity, and spatial demographic data like population density.9
With these large datasets, platforms conduct predictive modeling.1 Combining statistical analysis and ML, predictive models can guide epidemic response approaches through trend and pattern recognition.1 Predictive modeling includes many subcategories, such as spatial modeling, disease forecasting, and risk prediction, which can enable localized tactics, anticipate spread, and allow focused prevention of disease, respectively.1

Image Credit: metamorworks/Shutterstock.com
Examples such as the RAPIDD Ebola Forecasting Challenge9 and EPIWATCH3 demonstrate the real-world benefits of such models. The AI open-source-based platform, EPIWATCH, uses analysis tools such as FLUCAST, ORIGINS, and EPIRISK to predict the severity of upcoming flu seasons and provide guidance on epidemic prioritization.3
Challenges and limitations of AI in disease detection
From a scientific perspective, many areas of molecular biology remain elusive and are, therefore, difficult to model. For example, host-pathogen interactions concerning host immune systems are a complex and challenging factor in epidemic spread and pathogen activity.7 The incorporation of experimental high-throughput data, such as sequencing, into AI and ML models would potentially address this deficiency.7
From a logistical standpoint, a major challenge facing these models during outbreaks is maintaining reliable and current datasets.9 With rapidly changing situations, skewed and out-of-date assessments of disease spread risk can occur.9 This is particularly challenging with quickly progressing diseases like measles or influenza, which require updates at least daily as opposed to slower pathogens like HIV.9
Further, data quality is often lacking at the earliest and arguably most important stages of an epidemic or pandemic.2 Under detection or inconsistent collection can restrict the quality of data on deaths, testing, and infection rates.2 Further, restricted initial data creates difficulties in training AI and ML models, further hampering platform development.2
Case studies: AI in action against recent outbreaks
As previously stated, the COVID-19 pandemic forced the already growing field of AI into rapid advancement within the public health space.
Feng et al. used a Suceptible-Exposed-Infectious-Removed (SEIR) model to predict epidemic peaks through specific categorization of infected and recovered individuals.5 Their method was successful in predicting epidemic scenarios in Wuhan and non-Wuhan areas due to population migration.5 This model was also able to assess the effectiveness of lockdown and containment protocols in the Wuhan area.5
Additionally, Pirouz et al. developed multi-linear regression and AI approaches to examine correlations between case numbers of COVID-19 and environmental conditions like humidity, average temperature, and wind patterns.6 This model was successful in determining patterns such as the rapid spread of the SARS-CoV-2 virus in April and August due to warm temperatures, low humidity, and low wind speed, which can then predict seasonal increases in infection.6
The future of AI in epidemiology
The field of AI and ML, in general, is a rapidly developing area, and the application of these tools in public health is still in the early stages.
Deep Learning is an extrapolation of the previously outlined AI and ML platforms that are in active development in public health applications and will likely play a major role in future endeavors.4 Containing levels that humans haven’t constructed, these methods have shown great promise within drug discovery and large-scale pharmaceutical efforts and are demonstrating the same within the public health space.4
Once established on a larger scale, the global use of AI tools with intercontinental cooperation could lead to establishments such as global epidemic monitoring centers and large-scale global epidemic forecasting.4 Such organizations could turn tides in future epidemics and pandemics by providing faster and more coordinated responses.4
Ethical considerations and data privacy
As cutting-edge AI platforms take root within public health, it brings significant regulatory and ethical concerns. With AI and data analytics come issues of privacy, transparency, and bias.
The use of patient data creates openings for violations of individual privacy. It will require robust regulation and patient de-identification if data such as electronic health records (EHRs) are involved.1 This can include compliance with the Health Insurance Portability and Accountability Act (HIPAA) within the United States and an awareness of bias and discrimination within the AI systems targeting vulnerable populations.1
Given these concerns and the many others actively being examined during this explosion of AI development, caution must be used in the implementation of these tools to avoid undue harm and unintended damage to the populations these platforms strive to protect.
Conclusion
AI is one of the fastest-growing topical developments in the tech industry, and its applications in the public health sphere are vast and plentiful. If executed properly and with care for ethics, AI and ML have the potential to transform epidemic surveillance and pathogen detection, creating better outcomes and saving lives.
References
- Olawade DB, Wada OJ, David-Olawade A, et al. Using artificial intelligence to improve public health: a narrative review. Frontiers in Public Health. 2023; 11:e1196397. doi:10.3389/fpubh.2023.1196397
- Wang H, Tao G, Ma J, et al. Predicting the Epidemics Trend of COVID-19 Using Epidemiological-Based Generative Adversarial Networks. IEEE Journal of Selected Topics in Signal Processing. 2022;16(2):276-288. doi:10.1109/JSTSP.2022.3152375
- MacIntyre CR, Chen X, Kunasekaran M, et al. Artificial intelligence in public health: the potential of epidemic early warning systems. Journal of International Medical Research. 2023;51(3). doi:10.1177/03000605231159335
- Stergiou KD, Minopoulos GM, Memos VA, et al. A Machine Learning-Based Model for Epidemic Forecasting and Faster Drug Discovery. Applied Sciences. 2022;12(21):e10766. doi:10.3390/app122110766.
- Feng S, Feng Z, Ling C, et al. Prediction of the COVID-19 epidemic trends based on SEIR and AI models. PLOS ONE. 2021;16(1):e0245101. doi:10.1371/journal.pone.0245101
- Abdullahi SB, Muangchoo K, Abubakar AB, et al. Data-Driven AI-Based Parameters Tuning Using Grid Partition Algorithm for Predicting Climatic Effect on Epidemic Diseases. IEEE Access. 2021;9:55388-55412. doi:10.1109/ACCESS.2021.3068215
- Wong F, De La Fuente-Nunez C, Collins JJ, et al. Leveraging artificial intelligence in the fight against infectious diseases. Science. 2023;381(6654):164-170. doi:10.1126/science.adh1114
- Marcus JL, Sewell WC, Balzer LB, et al. Artificial Intelligence and Machine Learning for HIV Prevention: Emerging Approaches to Ending the Epidemic. Current HIV/AIDS Reports. 2020;17(3):171-179. doi:10.1007/s11904-020-00490-6
- Desai AN, Kraemer MUG, Bhatia S, et al. Real-time Epidemic Forecasting: Challenges and Opportunities. Health Security. 2019;17(4):268-275. doi:10.1089/hs.2019.0022
Further Reading
link